No Widget Added
Please add some widget in Offcanvs Sidebar
+91 7835973793info@graciousivf.com159- Second Floor, Keshav Vatika - Surya Nagar Phase 2, Sector 91- Faridabad 1210013
Please add some widget in Offcanvs Sidebar

In the IVF laboratory, after the egg retrieval procedure, fertilization is carried out by IVF (In-vitro fertilization) or by ICSI (intra-cytoplasmic sperm injection) and the resulting embryos are placed in an incubator for further development. The stages of development are as follows:
The blastocyst contains two different cell types- the inner cell mass which develops into the fetus, and an outer layer of cells called trophectoderm which develops into the placenta.
Historically, embryo transfer following IVF or ICSI has been carried out on Day 2 or Day 3 after egg collection. However, advances in the IVF laboratory advances allow us to now culture embryos for five or six days. This gives the embryos more opportunity to prove their developmental potential.
Some embryos stop developing (arrest) prior to day 5/6. This ‘natural selection’ enables the embryologist to identify and choose the best embryo/s for embryo transfer.
Blastocyst culture requires optimal laboratory conditions. On an average, about 45% of fertilized eggs reach the blastocyst stage. As only the embryos with the best development capacity become blastocysts, allowing embryos to grow and develop in the laboratory till they reach the blastocyst stage allows the selection of the most competent embryo/s for embryo transfer.
Blastocyst culture is advised for: For patients with multiple failed IVF: Performing a blastocyst culture on a patient with a history of failed IVF with day2/3 embryo transfer, can yield more information related to the growth of the embryos and aid in improving pregnancy rate To eliminate multiple pregnancies: Blastocyst culture allows the possibility of transferring the single best embryo and thereby reducing the chance of multiple pregnancy.
Not all clinics perform blastocyst culture. Quality control and optimal laboratory culture conditions are essential for successful blastulation.
There is a risk that none of the embryos become blastocysts. In that case the embryo transfer procedure gets cancelled. In good IVF laboratories, this usually means that probably none of embryos were competent enough to reach blastocyst stage and performing a day3 transfer also probably would not have led to a pregnancy.
Since fewer embryos become blastocyst, there maybe fewer or no surplus embryos to freeze after the initial embryo transfer in the fresh cycle. But, since success rates are better with a blastocyst transfer than with day3 transfer, a frozen may not be needed after all.
Should all patients go ahead with a blastocyst transfer?
Depending on factors like age, medical history and number and quality of embryos, it may be better to transfer a day3 embryo, particularly for women in their first IVF cycle.
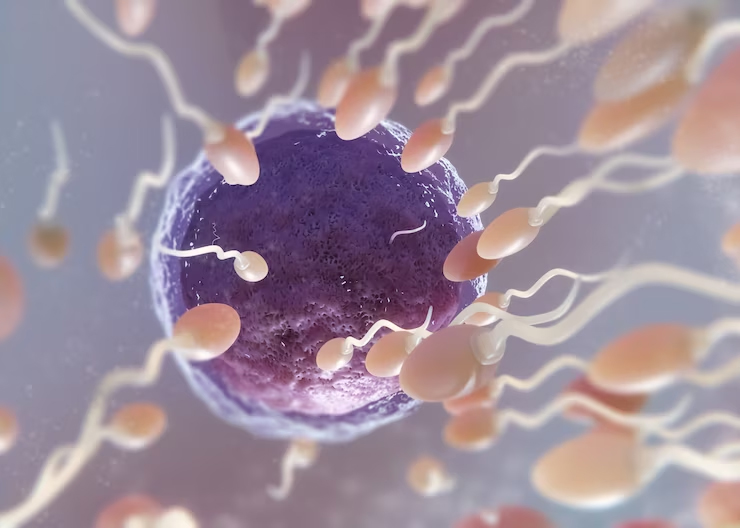
IVF (In vitro fertilization) is a process of fertilization where egg is combined with sperm outside the human body.
Read More
A tiny needle is used to inject at the centre of egg. As compared to ivf, IVF- ICSI has higher success rate.
Read More
Hysteroscopy: It’s a diagnostic tool to check that your uterus is healthy to carry your pregnancy or not and also fixes the problem.
Read More
Minimal Invasive surgical procedure to examine pelvic reproductive organ and pelvic cavity
Read More
IUI is a simple and affordable procedure in which our expert doctors put well prepared semen directly into the uterus to increase the chances of pregnancy.
Read More
This is a scientific IVF technique that can make it easier for the embryo to “hatch” or breakthrough its outer layer or “shell” (a membrane also known as the zona pellucida) by creating an opening.
Read More
Embryo freezing (cryopreservation) freezes and stores fertilized eggs for later use. It also can help people preserve fertility and get pregnant in the future.
Read More
A blastocyst is a cluster of dividing cells made by a fertilized egg. A blastocyst forms about five to six days after a sperm fertilizes an egg.
Read More